- September 10, 2019
- By Chris Carroll
The flight had been planned for years and rehearsed for months, but only a tragedy could set it in motion. On a Thursday in mid- April, the call came.
“We have a match.”
The caller was Dr. Joseph Scalea, an organ transplant surgeon at the University of Maryland Medical Center (UMMC) in Baltimore and an assistant surgery professor at the University of Maryland School of Medicine. For the last three years, Scalea—youthful, animated, with a crushing handshake and penchant for whoops and fist pumps—had been pouring enormous energy into a project that, if successful, could substantially change his field of medicine.
On the other end of the call was Tony “Pooch” Pucciarella, then-director of operations at the UMD Unmanned Aircraft System (UAS) Test Site in St. Mary’s County. An aerospace engineer and retired U.S. Navy pilot who’d flown both heavily armed maritime patrol aircraft and passenger planes, Pucciarella is as laid-back and circumspect as Scalea is exuberant.
That night—working with a team of more than 100 doctors, UAS Test Site aviation experts, organ transplant technicians and planners, police and other city and federal officials—they planned to remove a kidney from a deceased organ donor, strap it beneath a specially designed drone along with a new system to monitor the organ’s health, and send it on autopilot 2.8 miles across southwest Baltimore to UMMC. There, Scalea and other doctors would transplant it into a patient with kidney failure—a frontier never before crossed in medicine and flight.
It would have been easier to drive the kidney to the hospital from the Living Legacy Foundation, a nonprofit agency that coordinates organ donations in Maryland. The point, however, was to show doctors and transplant system officials that Scalea’s vision of national, on-demand organ shipments using drones to speed up transport and improve surgical outcomes wasn’t fundamentally bonkers.
“I’ve brought this up and been laughed out of the room,” he says. “They would literally laugh me out of the room.”
For the idea to be taken seriously, the UAS Test Site crew would have to engineer a rock-solid, reliable unmanned aircraft that wouldn’t fall out of the sky at the first hint of trouble and pulverize the precious kidney, or someone below. An equal challenge was finagling flight details over a densely populated area with Federal Aviation Administration officials dealing with a rising tide of civilian drones by enforcing strict rules about what could fly where and when.
As the doctor and the drone expert spoke on the phone, the gravity of the flight settled on them. A failed experiment might end not only Scalea’s hopes for the new system, but also a woman’s chance at survival. With uncharacteristic trepidation, he told Pucciarella, “I know you’re not going to let anything happen.”
After the call, Pucciarella’s wife observed he’d turned pale.
“I’ve done a lot of crazy things in military aviation, but this was pretty intense,” he said later. “There was a lot riding on this.”
THE PATIENT
 By early 2019, Trina Glispy of Baltimore realized she was likely to die as her father did, of kidney and heart failure.
By early 2019, Trina Glispy of Baltimore realized she was likely to die as her father did, of kidney and heart failure.
Glispy, 44, was in her mid-30s when her own kidneys stopped working. In 2011, she began dialysis treatments, hooking up to a machine three times a week, four hours apiece, to filter waste and toxins from her blood. She quit her job as a certified nursing assistant at the Baltimore VA Medical Center two years later.
“It was harder and harder to keep up with the patients,” Glispy says. “When you’re on dialysis, it’s just draining. It seems like it takes up most of your life.”
Glispy’s daughter, the oldest of four children, took over as the family’s primary breadwinner, while Glispy joined the national kidney transplant waitlist and arranged her life around the cycle of dialysis. If she missed an appointment or just had a bad week, fluid buildup made it hard to breathe and sapped her remaining strength.
She slowly climbed the waiting list, but three times in 2018 and 2019, possible matches fell through.
“I started to feel like I wasn’t going to get the kidney,” she says.
Scalea had already talked to her about the drone project, and Glispy agreed to participate. It sounded odd—the idea of a pilotless little helicopter buzzing over the city with her new kidney—but exciting as well. Glispy, who worked for years with military veterans at the VA hospital, was happy the flight would be overseen by two former military officers—Pucciarella and his boss, UAS Test Site Director Matt Scassero, a retired Navy captain.
Scalea asked Glispy once more just before the transplant whether she was still comfortable with the plan. Bring on the drone, she said.
THE PROBLEM
A clock starts ticking when an organ is separated from the bodily systems supporting it. If Glispy’s procedure went smoothly, only a few hours would pass between the removal of the kidney from the donor and its transplantation, improving her chances of a successful surgery.
“A kidney can last 24 to 30 hours on ice with a pretty reasonable outcome,” Scalea says. “After that, the results become a little shaky, because the organ is deteriorating.”
The creeping pace at which organs reach their patients regularly frustrates transplant surgeons. Ironically, medical advances contribute to the delays, because as doctors and transplant system officials increasingly gain the ability to precisely match organs to recipients, they cast a wider geographical net, upping the likelihood of a match thousands of miles away.
The organs’ journeys are coordinated by the equivalent of travel agents who struggle to rush the organs through crowded airports, or to and from areas poorly served by airlines. Another option is charter flights, but they can be expensive and complex to arrange.
“Here in Baltimore, we’re blessed to be served by a very active airport, but in many parts of the country where that’s not the case, we struggle to get kidneys onto commercial flights to reach waiting recipients,” says Charlie Alexander, CEO of the Living Legacy Foundation, which worked with the grieving family that entrusted a loved one’s organ to the University of Maryland drone.
Alexander, a former trauma nurse at UMMC’s R Adams Cowley Shock Trauma Center, wants to avoid an even more distressing outcome: “I can recall three events when organ recovery teams went down on charter flights or helicopters doing this work. If we didn’t need to have people on those missions, those losses wouldn’t have to happen.”
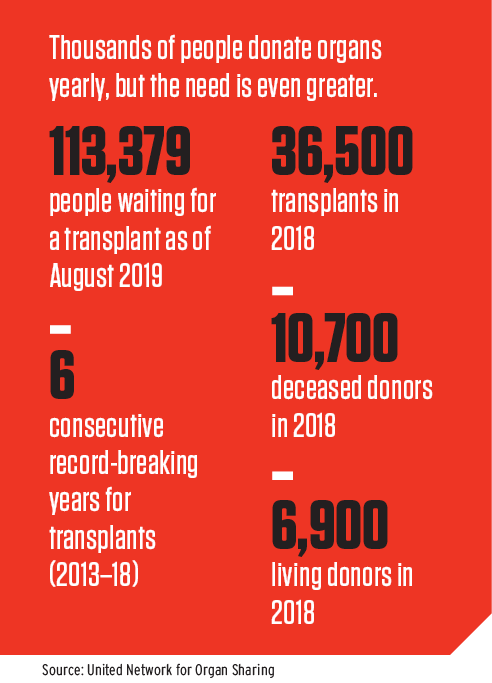
The upshot of the difficulties of moving organs is that in 2018, about 4% of kidney transports directly overseen by the United Network for Organ Sharing, which manages the organ transplant system nationwide, had unexpected, multi-hour delays, and 1.5% didn’t reach the destination in a usable state. Scalea once implanted a kidney that had taken 29 hours to make it from Alabama to Maryland, potentially reducing the lifespan of the organ by years.
“I thought to myself, this is completely crazy—we have incredible technologies at our fingertips, and we can’t even get a lifesaving organ from one place to another in a timely fashion,” he says.
THE PARTNERSHIP
 In 2016, while discussing the problem with Alexander and thinking about technological solutions, Scalea landed on an idea for a web of small, fast, relatively inexpensive drones to speed organs between nearby hospitals or cross-country to supplement the current delivery system. Meanwhile, a suite of sensors would constantly monitor temperature, vibration and other variables, and a GPS tracking device would ensure the aircraft could be found if it went off course or crashed.
In 2016, while discussing the problem with Alexander and thinking about technological solutions, Scalea landed on an idea for a web of small, fast, relatively inexpensive drones to speed organs between nearby hospitals or cross-country to supplement the current delivery system. Meanwhile, a suite of sensors would constantly monitor temperature, vibration and other variables, and a GPS tracking device would ensure the aircraft could be found if it went off course or crashed.
Although an ambitious plan, Scalea realized it could make individual transplants “faster, safer and cheaper,” he says, and benefit patients by ultimately making more organs available for transplantation.
Drones have risen in the public consciousness over the past decade as government agencies increasingly used them in military operations and disaster recovery. Amazon, Google and other companies, meanwhile, are exploring fast, automated package delivery by unmanned aircraft. Smaller, cheaper variants have become popular with hobbyist pilots.
Scalea called Norman Wereley, chair of the A. James Clark School of Engineering’s aero-space engineering department. Organ delivery might turn out to make the UAS an indispensable part of the medical system, Wereley said, and he put Scalea in touch with Scassero at the engineering school’s UAS Test Site.
The director at the test site, Scassero spent three decades in the Navy as a flight officer with a background in electronic warfare, serving in combat in Operation Desert Storm and the Kosovo War.
The two quickly devised a project that was later partly funded by the MPowering the State strategic initiative, which leverages complementary strengths at UMD and the University of Maryland, Baltimore, including the University of Maryland School of Medicine.
Scalea’s idea seems straightforward, Scassero says, but contains hidden challenges.
“Technically, to go from point A to point B carrying an organ isn’t that hard,” Scassero says. “But to do it with complete reliability, in a way that the FAA and the medical community will both have confidence in—that’s a challenge.”
THE DRONE
To carry a lifesaving organ to one of Scalea’s patients, the aircraft design would have to proceed less like a typical civilian drone, and more like a civilian passenger plane, with redundant safety systems.
Scassero assigned test site aerospace engineer Luan Duong ’13 to design what they would call the LG-1000. Flight had fascinated Duong since he began flying model planes as a boy with his father in Vietnam, and after immigrating to the United States, he chose the Clark School’s aerospace engineering program, gravitating to unmanned aircraft.
“When you work on a larger aircraft, you design a part on a computer,” he says. “When you work on a drone, you can design the entire aircraft, then get your hands dirty when you build it.”
Most civilian drones are, Pucciarella says bluntly, “a big bundle of single-point failures,” each capable of creating a catastrophic failure. To make their drone more resilient, Duong selected an eight-rotor design rather than the more typical four-rotor configuration, allowing the drone to continue flying even if a motor or two died. A battery failure would send a typical drone hurtling toward the ground, but this one would use a pair for backup. Two radios would guard against a loss of communications. And if everything else failed, Duong had a last resort.
“Tony called me up and said, ‘Hey, you gotta buy a parachute,’” Scalea says. “I just laughed … but then I was like, ‘Yeah, we should definitely have a parachute.’”
The drone underwent 44 test flights including a final one along the actual route in Baltimore in April.
Then the team settled down to wait for Glispy’s kidney match.
THE FLIGHT
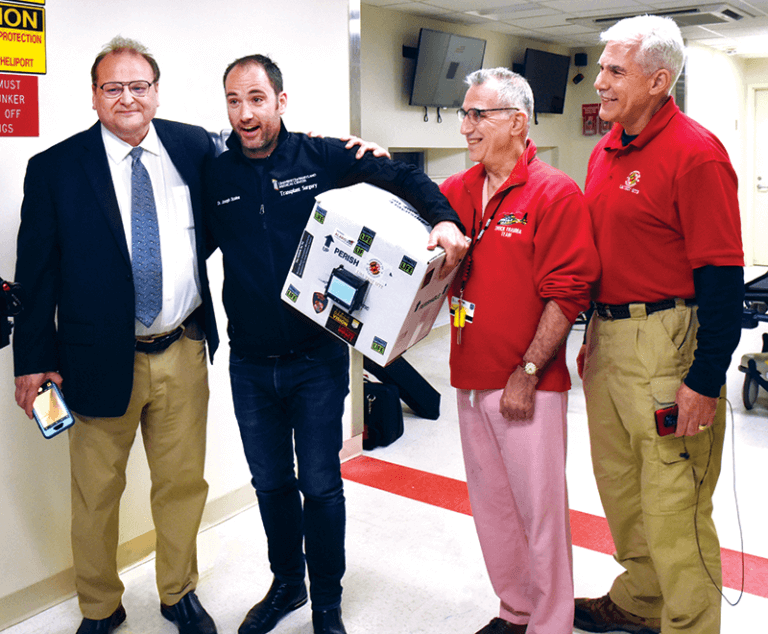 In the early hours of April 19, some team members gathered in a parking lot near Baltimore’s St. Agnes Hospital, while others waited at UMMC. Scalea, Scassero and Alexander marked the occasion with brief remarks about Glispy’s bravery in allowing her lifeline kidney to be used in the experiment, and praised the deceased donor and grieving family for the gift of life.
In the early hours of April 19, some team members gathered in a parking lot near Baltimore’s St. Agnes Hospital, while others waited at UMMC. Scalea, Scassero and Alexander marked the occasion with brief remarks about Glispy’s bravery in allowing her lifeline kidney to be used in the experiment, and praised the deceased donor and grieving family for the gift of life.
After strapping the standard, cardboard organ delivery box holding the kidney and monitoring system to the drone, Scalea jumped into a Baltimore police car and raced toward UMMC while BPD officers shut down streets along the flight path. Because the FAA certificate of authorization for the flight required it to always remain in sight, UAS Test Site personnel fanned out along the route to keep an eye on the drone as it passed 300 feet overhead.
As soon as Scalea arrived at the hospital, Pucciarella gave the launch order, saying, “Let’s make some history.” As it rose into the night sky, he removed his cap and crossed himself.
The team was confident in its UAS, but less so in one variable that members couldn’t control. Because it was supposed to land on the busy Shock Trauma helipad, any incoming emergency medical flight would bump theirs. If notification came early enough, the aircraft could double back, get fresh batteries and try the approximately 20-minute flight again. After a certain point, however, the remaining battery life would force it to continue on, and if the pad was still occupied, test site engineer Josh Gaus ’18, waiting at the hospital, would have to manually land it on a regular rooftop—doable, but riskier than the pad.
But the drone was cleared to proceed, and as it landed atop Shock Trauma, wild cheers erupted from the small crowd that had gathered. Pilot Ryan Henderson declared the drone “disarmed,” and Scalea crouched next to it to peer at the digital readout on the box containing the organ.
“Temperature is appropriate, organ doesn’t appear to be injured at all—looks like a perfectly transplantable organ,” he said, clearly fighting to control his excitement.
THE FUTURE
 Two months after her surgery, Glispy said her recovery has had its up and down days, but all of them are better than dealing with the endless grind of dialysis and constantly feeling that her time was running out.
Two months after her surgery, Glispy said her recovery has had its up and down days, but all of them are better than dealing with the endless grind of dialysis and constantly feeling that her time was running out.
“I don’t feel like my life is on a clock anymore,” she said, adding that she hopes to return to work as a nurse’s assistant soon.
Scalea, Scassero and Pucciarella are now discussing further organ delivery flights around the country, including in cities with desert and high-altitude environments. How the eventual system will be built, and with what kind of drone, remain uncertain.
The research Scassero and crew are conducting at the UMD UAS Test Site could help answer broader questions: How does the industry go about creating a supply chain of reliable aircraft components, much like in passenger aviation? What complex technical and policy adjustments are needed to integrate drones into U.S. airspaces on a regular basis?
They’re problems that must be solved before Scalea’s dream of a speedy, nimble transport system can whisk lifesaving organs from city to city, or across the continent.
“Basically, I can’t wait to be able to tell my patients they’re going to get several more years of life out of their organs because of how we transplanted them,” he says. “This is my passion. I believe I can really help my whole field, and do it with this incredibly talented group of smart people at the University of Maryland.”
Topics
Research