- July 07, 2025
- By Emily C. Nunez
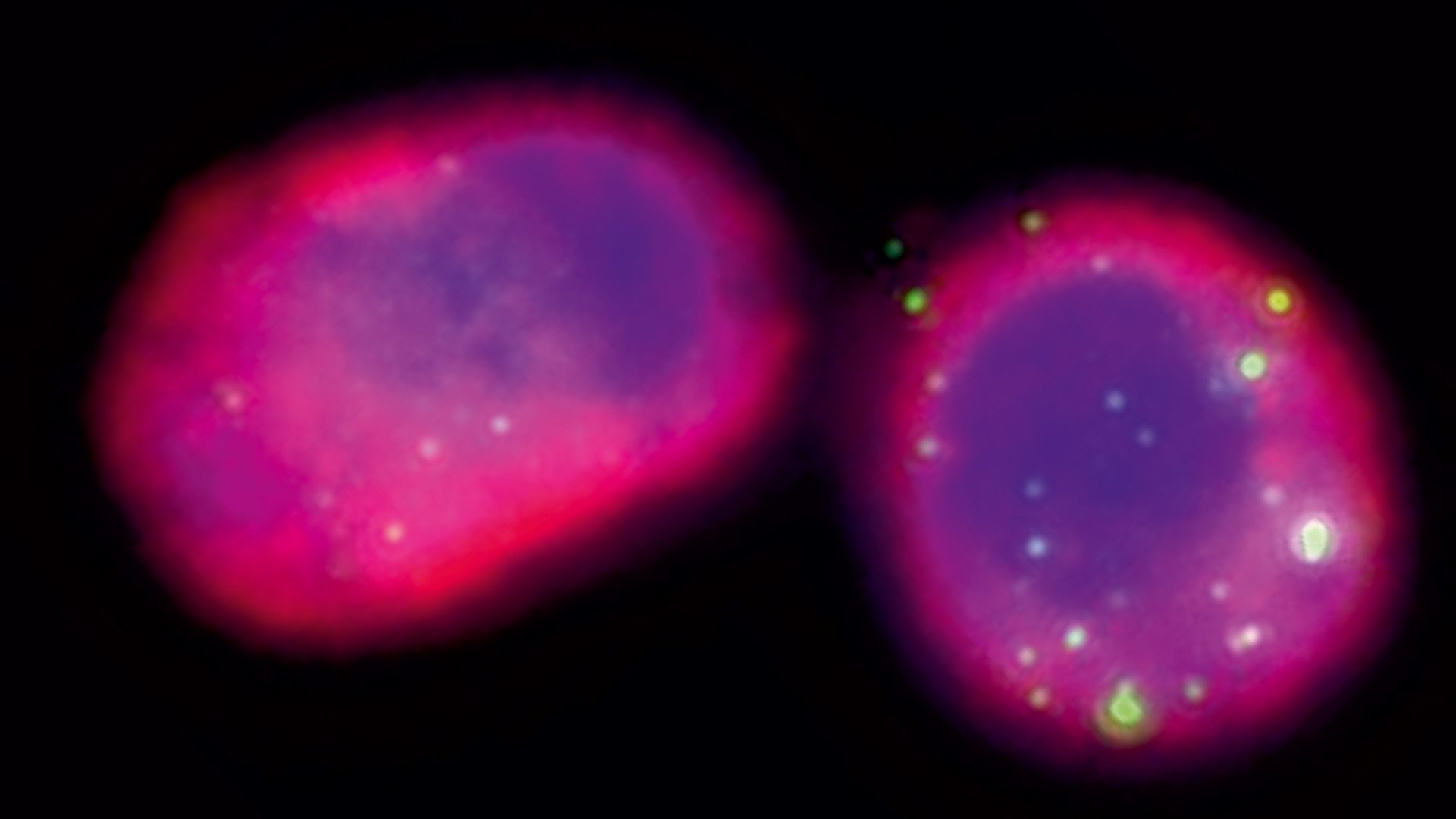
Antibiotic-resistant infections are on the rise, and some in the medical community are turning to bacteriophages—viruses that exclusively target bacteria—for backup. A new study co-led by a University of Maryland biologist sheds light on the complex interaction between bacteriophages and the immune system, finding that in some cases, mechanisms in the body that normally prevent infections might also fight off help from these “good” viruses.
Published July 1 in the journal Nature Communications, the study by the teams of Professor Joshua Weitz at UMD and Laurent Debarbieux at the Institut Pasteur in France, assessed the effectiveness of phage therapy in treating pneumonia. Their discoveries about the mechanisms behind phage therapy could one day lead to more individualization of treatments for patients facing these deadly infections.
“There is an increasing number of bacterial infections for which antibiotics fail, leading to worrisome projections of very large numbers of hospitalizations and fatalities because we're running out of options to treat multi-drug resistant superbugs,” said Weitz, who is also affiliated with the University of Maryland Institute for Health Computing (UM-IHC).
In their study, the researchers introduced phage to animal models to investigate their effectiveness in alleviating an acute pneumonia infection caused by Pseudomonas aeruginosa, a bacterium that lives in natural environments and leads to tens of thousands of hospitalizations and thousands of fatalities annually in the U.S. alone.
“In a therapeutic context, phage diffuse and come into contact with bacterial pathogens,” said Weitz, the Clark Leadership Chair in Data Analytics. “The premise of phage therapy has been that adding phage that specifically target and kill pathogenic bacteria can lead to infection clearance, but the reality is more complicated.”
In a test tube, phage and bacteria contacts can lead to a rapid collapse of the bacterial population. In contrast, in an animal or human host, the proliferation or collapse of a bacterial population depends on the efficiency of phage killing and the response of the immune system. Ultimately, this “immunophage synergy” is pivotal for the success of phage therapy, Weitz explained.
The experiments showed a surprising complication: Immunocompromised animals with depleted levels of alveolar macrophages—the most abundant immune cells in the lung that serve as critical first responders to infection—responded better to phage therapy than those with normal levels.
Debarbieux said they initially expected that all immune cells would work with phage to tackle the infection.
“While alveolar macrophages are protecting the lungs from pathogens, their presence surprisingly hampers the efficacy of phage therapy,” Debarbieux said.
To understand why, the researchers used in vivo experiments performed by first author Sophia Zborowsky and colleagues at the Institut Pasteur and a mathematical model developed by Weitz’s group to represent the feedback between immune cells, bacterial pathogens and therapeutic phages.
Former Weitz group postdoctoral associate Jeremy Seurat, the study’s first co-author, and UMD biology postdoctoral associate and study co-author Jacopo Marchi designed this model, which revealed that alveolar macrophages were depleting the phages and lowering their chances of reaching bacteria.
The findings suggest that physicians will someday be able to include personalized data on a patient’s immune system to better tailor the use of phage therapy.
“Moving forward, this research may help inform the eligibility criteria of patients and design therapeutic strategies to leverage the positive while avoiding the negative feedback of immunophage synergy,” Weitz said.
The next steps of this research could involve building predictive models to better estimate the effectiveness of phage therapy under different conditions.
Topics
Research